What is Keratoconus?
Normal cornea
Keratoconus
Keratoconus is a disorder in which the shape of the cornea changes, myopia and irregular astigmatism intensitfy, and as it progresses, it cannot be corrected even with glasses or contact lenses, and corneal transplantation is required.
The cause is unknown and it is a congenital, progressive disease. Eye-rubbing irritation (corneal abrasion) such as atopy and allergic disease is said to be an exacerbating factor, but it may develop without such an incentive.
There are no subjective symptoms in the initial stages. As the disease progressive, astigmatism increases, but good corrected visual acuity can be achieved with glasses or contact lenses. Therefore, it is rarely detected in the early stages in most case and is generally detected after detailed analysis of corneal shape by means of testing such as for refractive surgery. Keratoconus develops in most people during adolescence in the second and third decades of their life, then progress, and become less likely to progress after the age of 40. Rarely, it is discovered after the age of 30 and progresses after the age of 50. It is said to affect 1 in 1,000 people, and it is not a rare disease.
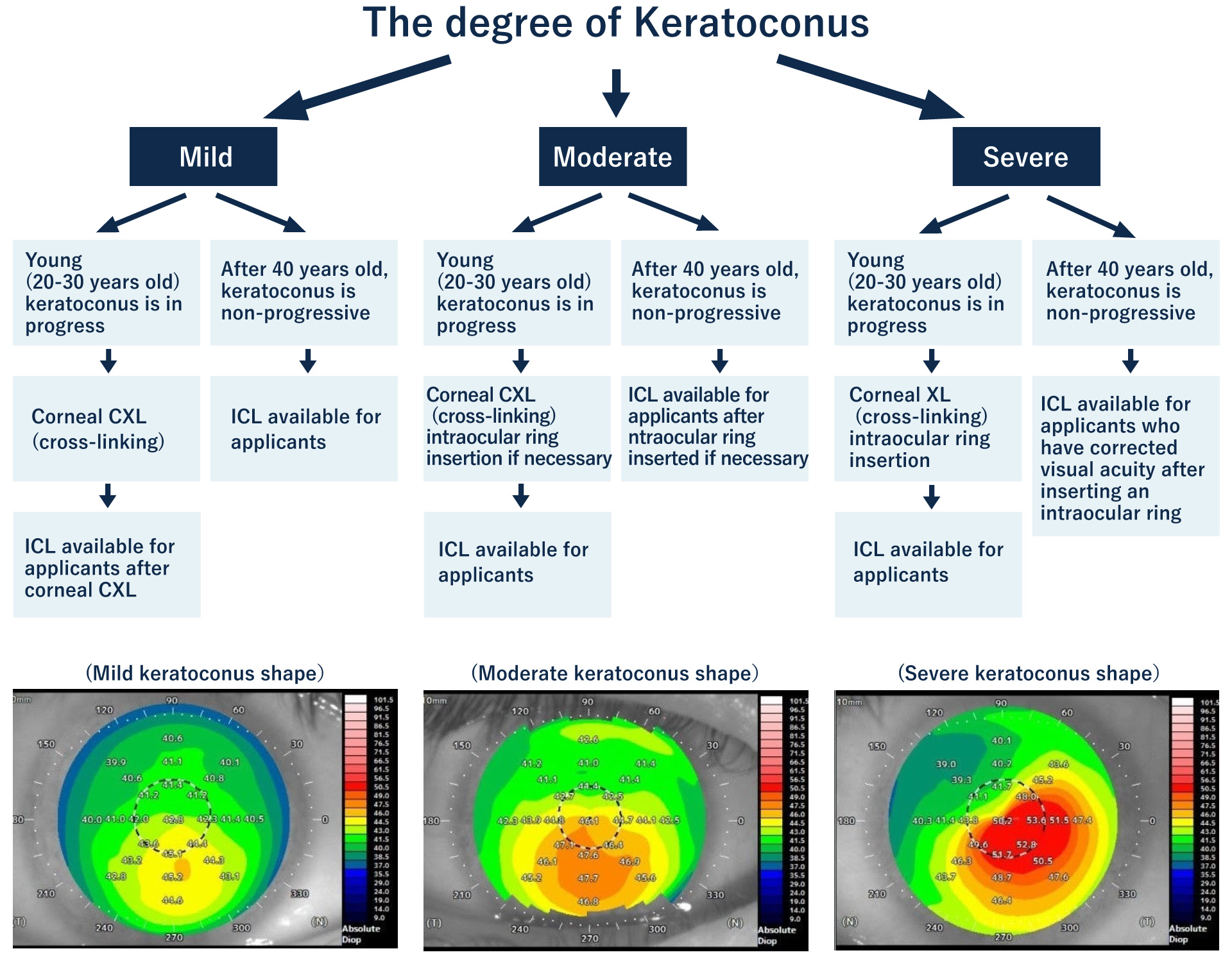
The treatment of keratoconus is different according to the development of cornea.
At Eye Clinic Tokyo, combining the treatment for keratoconus and ICL is suggested to greatly reduce the degree of myopia and astigmatism in those with stable corrected vision and thicker cornea than specified.
In February 2019, the Japanese Society of Ophthalmology revised the “guidelines for refractive orthodontic surgery (7th Edition)”, “previously considered to be contraindicated” for keratoconus cases in the treatment of ICL. Now the possibility of treatment has expanded. Kitazawa, who is in charge of the operation, is certified as an ICL expert instructor, with only ten people in Japan having this certification, and has rich experience with respect to providing patients with world-class treatment.